What is a fall? It depends on whose definition you use. The World Health Organization (WHO) defines a fall as…“an event which results in a person coming to rest inadvertently on the ground or floor or other lower level.”
An accurate definition of falls includes any uncontrolled descents onto any surface. How about that plop onto the bed or into the wheelchair? This could be a precursor to a fall. Does the person have impaired balance or muscle weakness? That could also be a fall waiting to happen.

Statistics on Falls
- One in three adults aged 65 and older falls every year.
- Falling doubles your risk of falling again.
- 30% of people who fall will end up with moderate to severe injuries related to the fall.
Falls are not a normal part of aging. Common reasons for falls include:
- Muscle weakness
- Environmental hazards
- Medication
- Poor footwear and foot care
- Vitamin D deficiency
- Low vision
Risk Factors for Falls
A fall history in the last six months is the most predictive factor of a future fall, along with intrinsic factors, including comorbidities. This is especially true if an individual is diagnosed with dementia, a hip fracture, diabetes, Parkinson’s disease, or arthritis. Cognitive impairment, acute or chronic condition, balance, gait, or visual impairment can also contribute to a higher fall risk, such as inappropriate footwear, dehydration, and peripheral neuropathy.
Falls and Wheelchairs
Wheelchair users demonstrating abnormal postures, such as a posterior pelvic tilt, have a high fall risk.
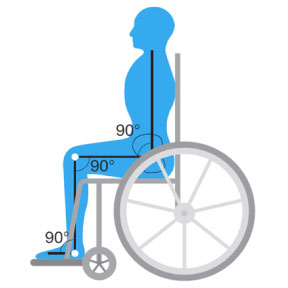
First, a clinician must ask, “What is causing the resident to sit in an unsafe manner?” Are they in a standard sling-back wheelchair? Are their hamstrings tight? Most people’s bodies cannot accommodate sitting 90°x90°x90°. It is like trying to fit a square peg into a round hole.
Rather than treating the symptoms, clinicians need to identify the cause of the abnormal posture, which is the key to preventing falls from the wheelchair. Common reasons for sacral sitting and sliding can be due to wounds, tone, discomfort/pain that is exacerbated using a sling seat.
What Not to Do!

- Don’t elevate the lower leg supports! This puts tremendous stress on the hamstrings, and it will be painful.

- Avoid the use of pommel cushions! The groin is not a weight-bearing surface.

- Never place non-slip matting directly underneath a person. Non-slip materials, such as Dycem®, are only for use under a cushion. Placing it on top of the cushion can cause shear, which results in instant, invisible skin damage. Think of it like this: cushion covers generally have a high coefficient of friction to assist in keeping someone in their seat. Dycem has a VERY high coefficient of friction. With Dycem, instead of sliding on the cushion, the pelvis is sliding under the skin!

- Avoid using the “dump” maneuver, which elevates the front of the chair by raising the front caster wheels. While “dumping” can decrease sliding, it will also create pressure over the ischial tuberosities (ITs). Patients will then experience pressure injury on the ITs instead of the sacrum. “Dumping” also creates shear risk.

- Remember that many patients with cognitive impairments will try to relieve pain and discomfort by attempting to stand, possibly placing them at risk for a fall.
Any highly effective intervention must be consistently followed outside of therapy (e.g., sit to stand from a chair for strengthening and pressure relief.). Make sure that the entire care team is on board with the intervention plan.
For more ideas on interventions for reducing fall risk, contact Broda by calling 844-552-7632 or email us at info@brodaseating.com.
References
- World Health Organization. (2021, April 26). Falls. Fact Sheets. Retrieved from https://www.who.int/news-room/fact-sheets/detail/falls
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. (2023, May 12). Facts About Falls. Retrieved October 19, 2023, from https://www.cdc.gov/falls/facts.html