In the realm of long-term care, the term “restraint” often sparks a heated debate among providers, therapists, and administrators. Restraints are any physical or chemical devices that limit a resident’s movement and cannot be removed by them without help. While restraints are not prohibited, rules do apply.
What are the rules for using restraints in long-term care?
If you need to use a physical restraint for a resident, you must:1
- Always use the least restrictive restraint for the least amount of time possible
- Provide ongoing re-evaluation of the need for the physical restraint.
- Never use a restraint for the convenience of the staff or as a form of discipline.
- Never use physical restraints to unnecessarily inhibit a resident’s freedom of movement or activity.
- Only use a restraint when a medical condition warrants the use of that restraint for the resident’s safety, wellbeing, and/or quality of life.
Did you know that the practitioner’s order alone isn’t sufficient documentation to warrant the use of a restraint? The physician’s order must be accompanied by supporting clinical documentation, clinical assessment, interdisciplinary care planning, medical symptom documentation, ongoing sign-off from the resident’s physician, and using the restraint for the least amount of time possible.1
The facility is accountable for the entire documentation process. Be certain that you are aware of your facility’s guidelines. If you’re not sure, check with your supervisor or clinical director.

What to Do in a CMS Survey to Avoid Tags
When your facility is being surveyed, you may wonder what the surveyor is considering when looking at restraint usage for your residents. If a surveyor notices a restraint, their goal is to determine if it complies with the regulations. They will use the following checklist to determine whether to cite a tag.
To be in compliance, the restraint:2
- Must be necessary to treat a medical symptom
- Must not be used to discipline a resident or for staff convenience in the absence of a medical symptom
- Must not be used because of family request in the absence of a medical symptom
- Must be the least restrictive device possible, in use for the least amount of time per day possible, and the facility must have an active plan in place to decrease usage or for eventual removal of the restraint.
If the sampled devices are found to be non-compliant, your facility will be under a much more thorough care area investigation and may receive a tag. Be aware that surveyors are not only checking your documentation but are also observing whether staff are consistently implementing this care plan over time and across various shifts.2 If you are a leader in your facility, make sure your team is aware of the importance of following care plans to the letter.
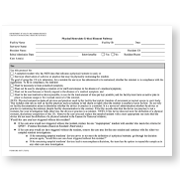
Physical Restraints Critical Element Pathway (HHS & CMS Form)
For a more detailed look at the surveyor’s process, here is the form that they use to evaluate correct use of restraints during a survey.
Examples of Potential Restraints in Long-Term Care
Restraints come in various forms, including seat belts, bed rails, trays, and even pressure alarms that make residents apprehensive about moving. However, it is crucial to understand that the main indicator of a restraint is its potential to restrict movement. This understanding guides the principles for their appropriate use:
- Seat Belts and Bed Rails: Typically used for safety but can restrict movement if misused.
- Trays: While helpful for meals, they can immobilize if the resident is unable to remove the tray themselves or if it remains in place unnecessarily.
- Pommel Cushions: Used to prevent sliding, yet they can act as restraints if the resident is unable to stand up from the wheelchair (and was previously able to do so before the use of the pommel cushion).
- Pressure Alarms: Intended to alert staff of potential pressure injuries before they form but can inadvertently discourage residents from moving freely due to fear of setting off the alarm while shifting their weight.
- Bedsheets: If sheets are tucked in so tightly that a resident cannot move, this is considered a restraint.
- Tilt Wheelchairs: Seat tilt lowers the user’s center of gravity and makes it difficult for the person to stand up from the wheelchair independently. Since tilt affects independent sit-to-stand transitions, it can be considered a restraint when not used to treat a condition and/or without documentation.


Why Facilities Hesitate with Wheelchair Positioning Devices
Many healthcare facilities hesitate to utilize positioning wheelchairs due to the fear of inadvertently using a restraint. The paperwork associated with restraints can be cumbersome, often requiring input from therapy, nursing, and support staff. Each facility has its own guidelines, and professionals must adhere to these, regardless of their personal views. This can lead to missed opportunities where positioning wheelchairs could significantly enhance patient comfort and mobility.
The Broda Tilt-in-Space Wheelchair
The Broda tilt and recline positioning wheelchair prioritizes patient welfare over restriction. Here’s why it’s not considered a restraint when used and documented properly:
- Therapeutic Necessity: When all other wheelchairs fail, and a thorough evaluation by therapy or nursing justifies its use, the Broda chair is essential rather than restrictive.
- Skin Integrity: Maintaining skin health is crucial for five-star ratings in facilities, and Broda’s design aids in preventing skin breakdown.
- Quality of Life: Quality of life metrics are pivotal, and positioning wheelchairs like Broda can alleviate pain and improve moods, enhancing these scores.

How Broda Wheelchairs Enhance Mobility and Quality of Life
Broda tilt-in-space wheelchairs provide a myriad of benefits that collectively enhance user mobility and quality of life:
- Fall Risk Reduction: By offering increased comfort and minimizing the need for frequent position changes, Broda chairs help reduce the likelihood of falls.
- Infinite Adjustability: The chairs are designed to adapt to the user’s needs, providing optimal support and positioning.
- Ergonomic Design: Features like low seat height, reverse mag wheels, and ergonomic self-propulsion enable users to maintain independence and better mobility.
- Patient-Centered: With a focus on comfort and ease, Broda chairs address common issues like pain and loss of sight lines, which can impede mobility and independence.
A Case Study in Effective Use
Consider a Huntington’s mid-stage resident who could still transfer independently. Initially, Broda recommended an Encore Pedal Wheelchair, but the facility was hesitant. The resident began sliding forward, prompting the therapist to suggest a pommel cushion—a restraint. By opting for the Broda tilt-in-space wheelchair instead, they provided effective support without compromising mobility, demonstrating its value beyond traditional solutions.
Psychological Harm from Incorrect Restraint Use
It’s important that clinical staff put themselves in the shoes of the resident at all times. Experiencing aging can be distressing – much more so if unnecessary restraints impact daily living.
Incorrect restraint use can cause:1
- Agitation & dangerous behavior
- Social withdrawal
- Depression
- Loss of dignity
- Shame
- Panic & anxiety
- Feelings of imprisonment or loss of freedom
These are sobering realities that should give anyone pause before using a restraint for a resident.
Psychological Benefit from Broda Wheelchairs
Although many restraints cause psychological harm, Broda wheelchairs have the opposite effect. Utilizing a Broda tilt and recline wheelchair not only enhances physical comfort and mobility but also fosters a sense of autonomy and dignity in residents, leading to improved emotional wellbeing and a reduction in feelings of frustration or helplessness.

Broda tilt wheelchairs also feature a front-pivot seat tilt. This means that unlike other tilt wheelchairs, the Broda wheelchair does not point a resident’s gaze at the ceiling. Rather, the rear of the wheelchair lowers into tilt on the front pivot point, allowing the resident to look directly forward, retaining a normal line of sight. Other seating solutions, such as Geri chairs and many other brands of tilt-in-space wheelchair, have a rear-pivot seat tilt, which raises the front of the wheelchair, forcing the resident to look upward. Maintaining a practical line of sight is a simple way that caregivers can provide dignity to their residents while also offering the benefits of reduced pain while seated.
Reducing pain improves quality of life. Over the 40+ years that Broda has been serving the long-term care industry, we have seen thousands of individuals become comfortably mobile after being confined to bed for months or even years. When residents are out of bed and engaging in activities of daily living, socialization, events, and more, they are much happier, increasing self-reported quality of life scores and overall family satisfaction.
Conclusion
Overall, by implementing the right wheelchair positioning device, health care facilities can improve their resident’s quality of life while adhering to the necessary guidelines for restraint use. So, it is highly recommended for long-term care facilities to consider investing in Broda wheelchairs for their residents’ overall well-being and satisfaction. Let us prioritize patient welfare over restriction and promote mobility and independence through responsible and effective use of restraints.
Learn more about how Broda can contribute to your long-term care needs. Contact a Broda Sales Representative today!
References
- Schrock, M. (2017, November 17). Physical Restraints F604. Columbia, MO; University of Missouri.
- Department of Health and Human Services Centers for Medicare & Medicaid Services. (2015, July). Physical Restraints Critical Element Pathway.






